Frequently Asked Questions
- 6-Month Deadline for Claims Submissions
- Fee-For Service (FFS) Payments
- Diagnosis Codes (ICD-9-CM)
- Microfilm Number & Claim Numbers
- Claims Submission Indicators
- Bilateral/Incision Indicator
- Number of Patients
- On-Call Indicator
- Pre-Authorized Indicator
- Special Circumstance Indicator (formerly called the “Split Indicator”)
- Workers Compensation Board (WCB) Indicator
- Personal Health Identification Number (PHIN)
- Start or Start & Stop Time
- Remittance Advice
Six (6) month deadline for claims submissions, including re-submissions
Q. What will happen to claims submitted past the 6-month time frame?
Manitoba Health (Health) provides coverage for insured medical services in accordance with The Health Services Insurance Act and its regulations. Section 4(2) of the Medical Services Insurance Regulation 49/93 states:
Payment to doctor
4(2) A medical practitioner who provides an insured medical service to an insured person, and who has not made an election under subsection 91(1) of the Act, shall submit to the minister:
(a) a claim for the service within six months from the date on which the service was provided in the form and manner required by the minister; and
(b) such further information respecting the service in a form and manner as may be required by the minister.
Claims (including re-submitted claims) received by Health more than 6 months after the service date will be rejected with Explanation of Benefits (EOB) code C2 This claim was refused as this service was not submitted within 6 months from the date on which the service was rendered.
All physicians are encouraged to submit claims on a weekly basis or at more frequent intervals to avoid late claim submissions.
The Medical Services Insurance Regulation does provide for an extension to the 6-month deadline for claim submissions, in extenuating circumstances:
4(3) The minister may extend the time referred to in subsection (2) if in the minister’s opinion there are extenuating circumstances that prevented the filing of the claim within the six month period.
Providers seeking an extension to the 6-month claims submission deadline are required to make the request in writing and include detailed information regarding the extenuating circumstance that prevented the submission of the claim to Health in accordance with the legislation, and addressed as follows:
Manager, Claims Unit
Fee-for-Service/Insured Benefits
Manitoba Health
3rd Floor, 300 Carlton Street
Winnipeg, MB R3B 3M9
Fee-For Service (FFS) Payments
Q. I receive paper cheques. Will I still receive paper cheques in the new claims processing system?
- Effective August 31, 2014, Health will no longer issue paper cheques for FFS payments. In preparation for this technological change and to improve claim system efficiency, all FFS payments will be issued through “direct deposit” or Electronic Funds Transfer (EFT).
- If you receive paper cheque(s), please complete the Practitioner Application for Electronic Funds Transfer
 form. This form must be completed and returned to Health by August 15, 2014 to ensure that you do not experience a disruption in your payments.
form. This form must be completed and returned to Health by August 15, 2014 to ensure that you do not experience a disruption in your payments. - Completed forms may be faxed to 204-942-2356, scanned and emailed to practitionerregistry@gov.mb.ca or sent by mail or courier “Attention Practitioner Registry” at the address on the form.
- Please note that even if you receive payment via EFT for some of your claim submissions, the enclosed form must be completed and returned with a void cheque to authorize EFT for all other payments issued.
Diagnosis Codes (ICD-9-CM)
Please Note:
- The requirement of a valid ICD-9 CM code affects MEDICAL (Physician and RN(EP)), DENTAL (Oral Surgery) and Optometric claims only.
- Optometric claims will continue to require the applicable optometric reason code in addition to a valid ICD-9-CM code. For example, 367 is no longer valid but 3670, 3679, 36720, 36721, etc. are currently valid ICD-9-CM codes.
- Chiropractors will continue to submit using chiropractic service codes. ICD-9-CM codes are not currently required for this provider group.
- Diagnosis Codes (ICD-9-CM)

Q. Where can I find the list of valid ICD-9-CM codes?
The source of valid ICD-9-CM codes used by Health can be found at:
www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes
- Health will not be converting to ICD-10 codes for medical claims at this time although the new system was built with the ability to use ICD-10 codes, if utilized in the future.
- posted Sept. 26, 2014
Microfilm Number & Claim Numbers
Upon the implementation of CPS, Health now assigns an 8-digit numeric microfilm number replacing the 2 alphabetic 6 numeric digit codes previously used.
Q. Will the microfilm number remain the same?
- Commencing with the implementation of the new CPS, Health will assign an 8-digit numeric microfilm number instead of the 2 alphabetic and 6 numeric digit codes now used.
Q. Are we still going to be required to put the claim number on operative reports and other documents submitted to support payment of the claim?
- Yes, all the usual information including the claim number, user site number, practitioner billing number, practitioner’s name, patient PHIN and registration number will have to be on the supporting paper documents submitted for all operative reports, by-reports, etc.
Claims Submission Indicators
Bilateral / Incision Indicator Field
Valid values for this field on the new CPS are as follows:
- B–Bilateral
- S–Same incision
- D–Different incision
- Blank–If not applicable to the line item
The Bilateral/Incision Indicator field must be blank when not applicable.
The Bilateral/Incision Indicator field should be used when submitting claims for procedures performed bilaterally (at the same sitting) and to indicate when multiple procedures are performed through the same or separate incisions. The use of this field without adding unnecessary remarks will expedite claims adjudication.
Q. If a claim is submitted for bilateral diagnostic imaging (e.g. X-ray of the ankles, hips or knees) will the “B” indicator be enough?
In CPS, the Bilateral/Incision Indicator provides supportive justification for benefits billed in multiples. When a procedure is done bilaterally, the B must be entered in the bilateral/incision indicator field in addition to the number of services being reported as 2. The addition of the B for bilateral services eliminates the need to record the words “bilateral” in the remarks section of the claim.
Q. If a claim is submitted for a repeat ankle X-ray on the same day (e.g. pre and post-operative), what fields should be populated? For example, an X-ray of a fractured ankle is performed at 1300 hrs and an X-ray of the same ankle performed again at 1530 hrs (post reduction).
In CPS, these types of radiology services should be billed on two different lines on the same claim with the different Start Times populated for each line. No remark to justify the two services is necessary. It is important to be aware that unnecessary remarks may delay processing time.
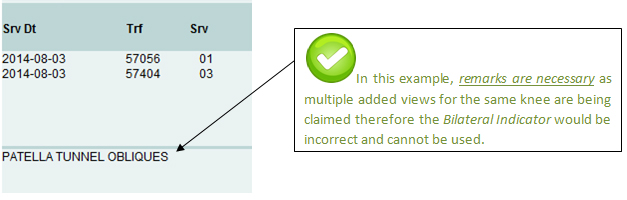
When is it necessary to include both the Bilateral/Incision Indicator and Remarks on a claim?
The use of the new fields in CPS, without adding unnecessary remarks will expedite claims adjudication.
Please see examples below:
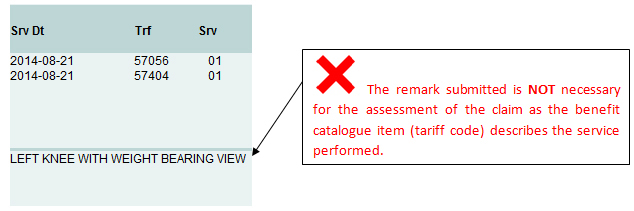
Scenario 1
This claim submission is incorrect:
Scenario 2
This claim submission is incorrect:
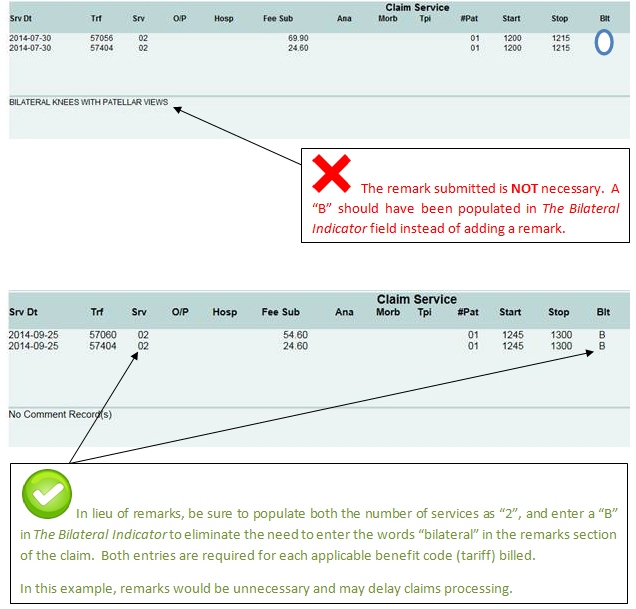
Scenario 3
The following benefit codes (tariffs) require the Bilateral Indicator, when applicable:
20114 |
21672 |
21829 |
25497 |
25843 |
57060 |
Number of Patients
Q. When is the Number of Patients Indicator required to be populated?
When submitting a claim for a group psychotherapy session or team conference, the number of patients must be entered in this field.
On-Call Indicator
Q. When is the On-Call Indicator required to be populated?
The On-Call Indicator field should be marked 'C' when a physician submits any fee-for-service claims respecting services rendered during the time when the physician is providing off-site, on-call/stand-by services pursuant to any of the following alternately-funded agreements which form part of the February 12, 2015 Master Agreement between Manitoba Health and Doctors Manitoba:
- Basic A & B
- Crisis Stabilization Unit
- Dauphin Psychiatric Unit
- Doctor of the Day
- HSC Pathologists
- NMU On-Call (Live-in Physicians Only)
- Obstetrics On-Call
- On-Call Specialist/Doctor of the Day
- Palliative Care Program Agreement
- Pathology On-Call
- Personal Care home On-Call
- Trauma Services
- Seven-Oaks Unassigned Patient
- Victoria General Hospital – Generalist Attending Physicians (GAPs)
Pre-Authorized Indicator
Q. When is the Pre-Authorized Indicator required to be populated?
The Pre-Authorized Indicator is used to report that the provider obtained prior approval from Health for coverage of a specific elective procedure (e.g. rhinoplasty, benefit code (tariff) 1950). This field should be populated with a “P” if the provider has received prior approval for coverage of the procedure. Inclusion of the Pre-Authorized indicator will expedite claims processing while failure to include it may result in incorrect claim adjudication.
Special Circumstance Indicator
Q. When is the Special Circumstance Indicator (formerly called the “Split Indicator”) required to be populated?
The Special Circumstance Indicator (formerly called the “Split Indicator”) will flag split claims for team surgeries, complete history and examinations done for hospital and CTU admissions, etc. The expanded values include the following:
- A – Admission (complete physical exam for admission to hospital).
- C – CTU (complete physical exam billed from CTU facilities 188, 201, 375, 380, 382, 383, 393, 394, 395, 396, 397 or 399).
- E – Used to indicate when the tariff chosen is similar or equal to another service found in the Physician’s Manual.
- G – General Anaesthetic – Used when a procedure with a fee less than the minimum fee listed in Note 2 (Physician’s Manual, Surgical Procedures, page D – 1) is done under general anaesthetic. The fee should be increased to the listed minimum and the G indicator added to the claim.
- H – Used when billing 78520 for supportive care. Please refer to Rule of Application 13–Supportive Care
- L – Used when requesting less than the standard benefit (tariff) rate or greater than the standard benefit (tariff) rate. Some examples are listed below:
- Rule of Application 40 – Where an Open Reduction is Followed by a Second Open Reduction by the same physician within the three (3) week period, 100% of the listed benefit will be paid for the first open reduction and 75% for the second reduction. The circumstances of the second requirement must be given by Special Report to justify this assessment.
- Benefit catalogue items (tariffs) with notes within the Physician’s Manual advising to submit at a reduced rate (e.g. 25105)
- Microsurgery add-on percentage to the basic fee.
- N – Used when requesting an additional 25% of the listed open reduction fracture benefit rate, for a demonstrated radiographic non-union. Please refer to Rule of Application 42 – Open Reductions.
- S – Split Surgeries – Rule of Application 30 – When Two Surgeons are involved in the management of a surgical case, by prior agreement between the surgeons; the total fee may be apportioned in relation to the responsibility taken and the work done. Each surgeon should send in his/her own claim showing the agreed apportionment to each surgeon.
- T – Triage – Used if the provider performs a complete physical exam of a patient in labour for possible admission.
Workers Compensation Board (WCB) Indicator
Q. When is the WCB Indicator required to be populated?
The WCB Indicator should be populated with a “W” if the benefit code (tariff) was originally submitted to WCB and denied and the benefit (tariff) is now being submitted to Health in one of the following circumstances:
- the claim is now past the 6-month claims submission deadline, or
- a child benefit (add-on) is submitted without the corresponding parent benefit (major procedure) because the parent benefit is being covered by WCB.
Failure to populate the WCB indicator when applicable may result in claims being refused with explanation of benefit code C2 – This claim was refused as the service was not submitted within 6 months from the date on which the service was rendered or, N1 – This service was refused as a “child” benefit catalogue item (add-on) cannot be claimed without the corresponding “parent” benefit catalogue item or if the “parent” benefit catalogue item is refused or rejected.
Personal Health Identification Number (PHIN)
Q. What patient demographic information is required in CPS?
- Every claim should have the following six (6) fields correctly completed for patient demographics:
- PHIN
- Registration Number
- Birth Date
- Gender
- Given Name
- Surname
The PHIN is a mandatory field on all claims. If the PHIN is not correctly entered on the claim, it will be rejected.
Q. Can a claim for a newborn be submitted without the PHIN?
- The PHIN is a mandatory field on all claims, including claims for services provided to newborns. If the PHIN is not correctly entered on the claim when it is submitted to Health, it will be automatically rejected.
- In CPS, claims for newborns submitted without a PHIN will be automatically rejected with the following Explanation of Benefit (EOB) code showing on their Remittance Advice: X5 – This claim was refused as the PHIN is: a) blank or b) invalid.
Q. How long does it take for a newborn to be assigned a PHIN by Health?
- Health can automatically register a newborn and assign a PHIN based on information provided directly from the Manitoba hospital where the child was born or from Vital Statistics.
- Most newborns are assigned a PHIN by Health within 7 to 10 business days of birth in a Manitoba hospital. The timeliness of the registration of a newborn can be impacted by the information received by Health from Vital Statistics, the hospital or the parent(s)/guardian(s).
- Please note that although a PHIN may be assigned to a newborn within a couple of weeks after birth, an updated registration card is not issued to the parent(s)/guardian(s) until they contact Health directly.
Q. Will the PHIN requirement in CPS affect the processing time for newborn claims?
- The PHIN is a mandatory field in the CPS. If the PHIN is not correctly entered on the claim when it is submitted to Health, it will be automatically rejected. Claims for newborns should not be submitted until a PHIN has been assigned.
Q. How is a newborn added to the Health Registry system and assigned a PHIN?
Newborn Information provided by a Manitoba hospital:
- When a baby is born in a Manitoba hospital, the mother is provided with a package of information, including Vital Statistics forms that may be completed either at the hospital before the mother is discharged or later at home.
- For births occurring at one of the larger centres in Manitoba (e.g. Winnipeg or Brandon), information is automatically generated from the hospital and sent to Health electronically.
- Health staff reviews the information provided by the hospitals for completeness and assign a PHIN to the newborn. If the information from the hospital is deemed to be incomplete, a PHIN will not be assigned. For example, if the newborn has not been named, a PHIN cannot be assigned. Likewise, if the mother’s last name does not match the child’s last name, a PHIN cannot be assigned until additional corroborating information is received via Vital Statistics.
Newborn information provided by Manitoba Vital Statistics:
- Vital Statistics receives information on newborns from the parents when they complete and submit the necessary forms to register their child and obtain a birth certificate. Every 2 weeks, Health receives an electronic report from Vital Statistics with information on babies born in Manitoba. Health can automatically assign a PHIN based on this information from Vital Statistics.
- Please note that although Health may assign a PHIN to a newborn within a couple of weeks after birth, an updated Health registration card is not issued to the parent(s)/guardian(s) until they contact Health directly.
Newborn information provided by the Parent(s) or Guardians:
- If information from either the hospital or Vital Statistics has not been received which would enable Health to automatically register the newborn for healthcare coverage and assign a PHIN, the parent(s) or guardian(s) must register the child by providing Health with a copy of the child’s birth certificate.
- Health’ ability to register a newborn for health coverage and assign a PHIN in a timely manner is impacted by the information provided by the parent(s) prior to discharge from the hospital or the information provided to Vital Statistics through completion of the required forms. The parent(s)/guardian(s) of a newborn who has not yet been assigned a PHIN should be directed to contact Health at the numbers below.
Q. How does a parent(s) or guardian(s) obtain a Manitoba Health card with their newborn added to it?
- In order for parents or guardians to obtain an updated card they must contact Health directly at 204-786-7101 or toll free at 1-800-392-1207.
- Updated Health cards are not automatically issued to new parent(s)/guardian(s). They must contact Health to request a new card.
- If Health has not received information from the hospital or Vital Statistics to automatically register the newborn for Health coverage, parents will need to provide Health with a copy of the child’s birth certificate.
- Parent(s)/guardian(s) can obtain a copy of the child’s birth certificate by contacting Vital Statistics at 204-945-3701 in Winnipeg; or toll free at 1-800-282-8069.
Q. Are there other ways for a practitioner to obtain a patient’s PHIN?
- iREG and eChart are two applications that are available to practitioners in Manitoba. Both applications provide access to the PHIN. Both applications offer different benefits that may have value for your practice.
- Physicians who would like to have more information about eChart should contact Manitoba e-Health at echartmanitoba.ca
- For more information about iReg, see the iReg release package on the WebLink applications main page.
- For practitioner offices that do not have eChart or iREG access, a 529 Form can be submitted to Health by fax to request patient demographic information, including PHIN.
START or START & STOP TIME
The use of the Start and Stop Time fields without unnecessary remarks will expedite claims adjudication.
24-Hour Format. “START” or “START & STOP” times must be entered in a 24-hour format, for example 11:30 p.m. is entered as 23:30. 24:00 and 00:01 are appropriate entries; however 24:01 or 00:00 are not valid start or stop times.
START TIMES
“START” times are required for:
- All benefits (tariffs) submitted on the same claim as an After Hours Premium benefit (tariff).
- All benefits (tariffs) submitted on the same claim as an Anesthesia Out-of-Hours Premium benefit (tariff).
- Submitting a claim for the following benefit codes (tariffs):
75550 75557 78005 78944 75553 75558 78474 78958 75555 78000 78486 79727 75556 78001 78576
- Second Visit/Examination on the Same Day: Individual “START” times are required when a patient is examined more than once on the same day. Without individual “START” times, the second visit will be rejected as a duplicate service.
- After Hours Premium (benefit codes (tariffs) 75550, 75553, 75555). All benefit codes (tariffs) submitted on the same claim as an After Hours Premium benefit (tariff) require a “START” time, regardless of whether a premium applies to that particular service.
- 1M – This claim was refused as the start time is: a) blank or b) invalid
- 3H – This claim was refused as start times are required for all services on a claim when an After Hours Premium or Anaesthesia Out-of-Hours Premium is being claimed. Please provide start times or submit any benefits that are not premium eligible on a separate claim.
- Z5 – This service was refused as the date of service or time of service does not correspond with the after or out of hours premium benefit billed.
- 41 – Benefit catalogue item has been returned unprocessed as it was submitted on the same claim as another benefit catalogue item that was rejected. This resulted in a full claim rejection. Please refer to the other EOB codes on this claim. Once corrections have been addressed a new claim may be submitted.
- Deliveries – After Hours Premiums. The time of delivery must be entered in the “START” time field for After Hours Premium and all services related to labour and delivery including obstetrical benefits for delivery, caesarean sections and benefits (tariffs) listed in the Physician’s Manual under the headings: Induction of Labour, Management of Complications of First and Second Stages of Labour, and Management of Complications of Third and Fourth Stages of Labour, as well as tariffs 4824 and 4826.
In cases where more than one special call is made on the same day for the care of an obstetrical patient, the time of each special call must be entered in the “START” time field instead of the delivery time for the special call benefits (tariffs) only, while any other benefits (tariffs) for services such as examinations, procedures and/or After Hours Premium require the time of the delivery.
NOTE: When submitting a claim with an After Hours Premium benefit (tariff) (75550, 75553, 75555), all benefits (tariffs) on the same claim require a “START” time, regardless of whether a premium applies to that particular benefit (tariff).
- Operative Procedures – After Hours Premiums. “START” times for After Hours Premiums must be entered based on the time the patient entered the operating theatre when billed in conjunction with operative procedures.
NOTE: When submitting a claim with an After Hours Premium benefit (tariff) (75550, 75553, 75555), all benefits (tariffs) on the same claim require a “START” time, regardless of whether a premium applies to that particular benefit (tariff). - Out-of-Hours Premiums (Anaesthesia benefit codes (tariffs) 75556, 75557, 75558)
All benefits (tariffs) submitted on the same claim as an Out-of-Hours Premium benefit (tariff) require a “START” time, regardless of whether a premium applies to that particular service.
If all benefits (tariffs) on the claim do not have a valid “START” time, the entire claim will be rejected automatically with one or more of the following EOB codes:
- 1M – This claim was refused as the start time is: a) blank or b) invalid
- 2H – This service was refused as the time given does not correspond with the number of services billed.
- 3H – This claim was refused as start times are required for all services on a claim when an After Hours Premium or Anaesthesia Out-of-Hours Premium is being claimed. Please provide start times or submit any benefits that are not premium eligible on a separate claim.
- Z5 – This service was refused as the date of service or time of service does not correspond with the after or out of hours premium benefit billed.
- 41 – Benefit catalogue item has been returned unprocessed as it was submitted on the same claim as another benefit catalogue item that was rejected. This resulted in a full claim rejection. Please refer to the other EOB codes on this claim. Once corrections have been addressed a new claim may be submitted.
If all benefits (tariffs) on the claim do not have a valid “START” time, the entire claim will be rejected automatically with one or more of the following EOB codes:
START & STOP TIMES
“START & STOP” times are required for:
- All time-based anesthetic procedural services.
- For all benefits (tariffs) submitted on the same claim as Detention and Transport benefits (tariffs).
- Submitting a claim for the following benefit codes (tariffs):
- Detention and Transport – Critically Ill Patient (benefit codes (tariffs)). All benefit codes (tariffs) submitted on the same claim as a Detention and Transport – Critically Ill Patient benefit (tariff) require “START & STOP” times, regardless of whether a premium applies to that particular service.
If all benefits (tariffs) on the claim do not have a “START & STOP” time, the entire claim will be returned with one the following EOB codes:
- 1M – This claim was refused as the start time is: a) blank or b) invalid
- 1N – This claim was refused as the stop time is: a) blank or b) invalid
| 22370 | 78572 | 78574 | 78632 | |
| 78565 | 78573 | 78630 |
Remittance Advice
Q. What is a Remittance Advice?
A Remittance Advice is the electronic information file that Health provides each pay period to assist you with reconciling your claims in your practice management systems. The remittance file is available for download from Health beginning on the 3rd business day after the electronic claim cut-off date until the next cut-off. Each remittance file must be downloaded by your billing staff.
The decision regarding the information you wish to extract from the remittance file should be made by you and your billing software vendor or service bureau. The list below shows the type of information that Health reports back to providers on the Remittance Advice file each pay period. If there are items in the list below that you would like to see on your reports, please contact your vendor to discuss.
The information included on the remittance file from Health is:
User Number
User Name
Practitioner Number
Surname (patient)
Initial (patient)
Given Name (patient)
Gender
Health Registration Number
Health PHIN
Health Microfilm Number
Claim Number (assigned by your system)
Health Identification Number for reciprocal/non-resident claims
Year of Birth
Non-Resident Birth Date (MMDD)
Practitioner Payment Option
Explanation of Benefit Code (EOB)
Incorporated Indicator
Referring Practitioner Number
Interest Amount
Hospital Code
Service Date (YYMMDD)
Prefix
Benefit code (tariff)
Number of Services
Province Code for reciprocal/non-resident claims
Fee Submitted
Fee Assessed
Manual Code
Location of Service
Medical Records Number, Clinic Number, or Provider's Patient Number
Q. Why should I check the Remittance Advice file?
It is critical to check your remittance file to determine whether or not your claims have been paid as submitted or if Health has reported an Explanation of Benefit (EOB) code to indicate that a claim has not been processed as submitted. The Remittance Advice also provides the status of claims that have been received by Health but not yet adjudicated (“pending”).
EOB codes have replaced the existing disposal codes found in the Physician's Manual. The EOB list is updated periodically with changes posted on this web page. In addition to the EOB description, an "action description" is also included for each EOB code. The "action" information is provided to assist practitioners and their billing staff in determining the appropriate action to take in response to the EOB code sent on the remittance file. The current EOB list is posted here  .
.
Please note: It is possible that not all of the “actions” listed will be accurate or appropriate for every unique claim situation, but rather, are meant to provide you with some guidance as to a possible action to take.
Q. What will happen if I do not check the Remittance Advice file?
Claims must be submitted to Health within 6 months of the date of service. If you do not check your remittance file on a regular basis, you may not have sufficient time to resubmit claims that have been rejected, reduced or changed within the required timeframe.
Health recommends that you submit claims as close to the service date as possible to ensure the claims are received within the 6 month timeframe.
Failure to reconcile the claims from your Remittance Advice in your system will also make it appear that a lot of claims are outstanding when in fact they have already been processed and may require further action.
Q. Where can I find the remittance advice?
Contact your vendor for more information relating to how to access your Remittance Advice information in your billing system.


